Retina Conditions Explained: Ocular Histoplasmosis
Presumed Ocular Histoplasmosis Syndrome (POHS) causes atrophy (wasting) around the optic nerve and multiple scars, called histo spots, in the choroid. These symptoms are accompanied by new blood vessel growth (neovascularization) that starts adjacent to a histo spot. Histoplasmosis is a disease caused by Histoplasma capsulatum (H. capsulatum), a soil fungus prevalent in certain parts of the American continent, in particular the Ohio and Mississippi River valleys.
Symptoms
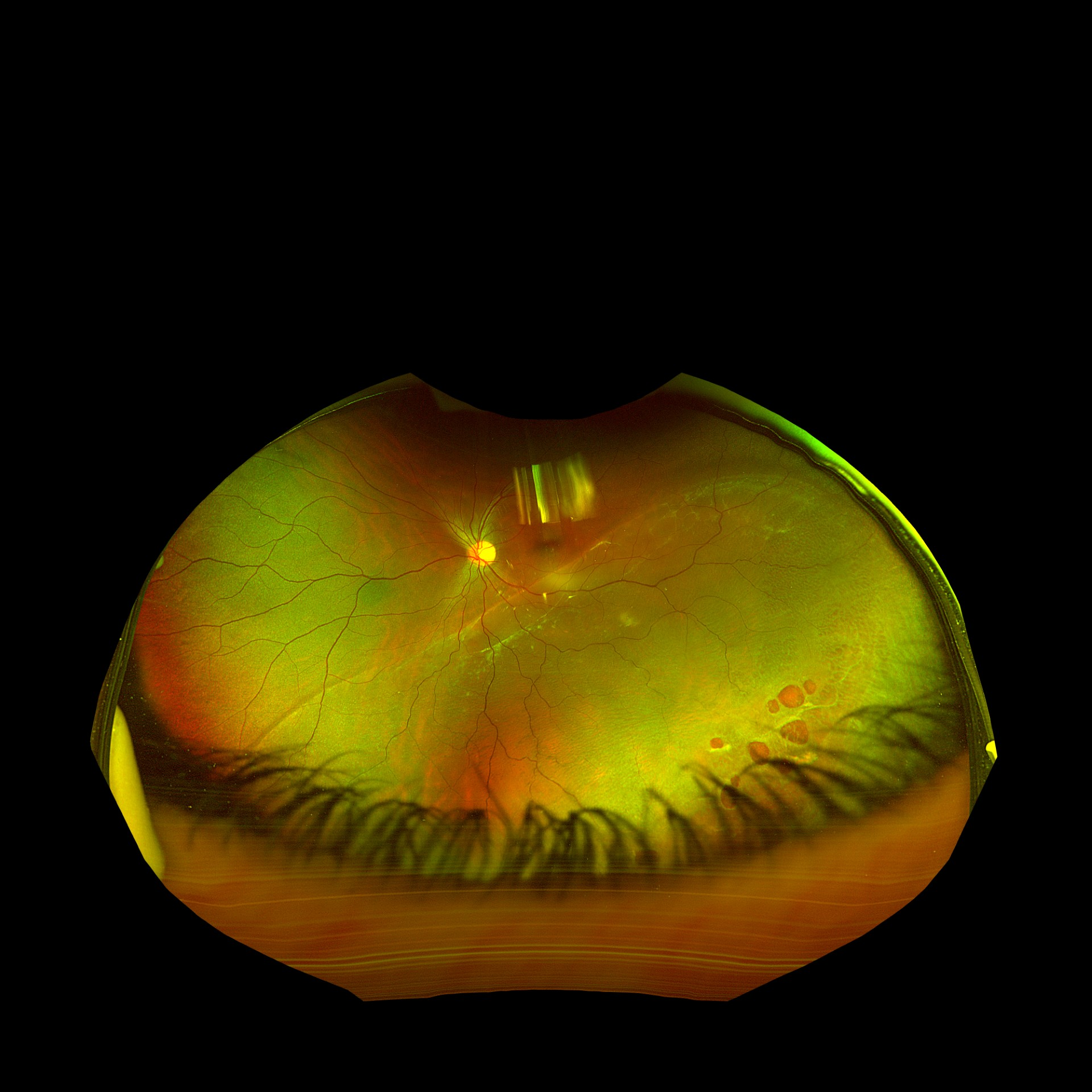
Histo spots (Figure 1) are considered the earliest stage of the disease. Less than 5% of individuals with histo spots will develop neovasculization in the central macula (at the middle of the retina). Because the histo spots themselves usually do not cause symptoms, patients typically do not develop symptoms until neovascularization grows in the central macula. Symptoms include painless, progressive blurring of central vision and wavy vision (metamorphosia), which can be sudden or develop slowly.
Treatment and Prognosis
Treatment is generally required only when there is neovascularization. Given that H. capsulatum does not seem to play a direct role in the development of POHS, antifungal agents are not used to treat POHS. However, injections of medications that inhibit neovascularization are recommended. These medications include bevacizumab (Avastin® ), ranibizumab (Lucentis® ) and aflibercept (Eylea® ). Prior to injection, the eye is given an anesthetic drop or gel and is cleaned with povidone iodine; the injection generally causes minimal, if any, pain. Injections are initially administered monthly until the neovascularization improves, as confirmed by OCT or FA. If neovascularization is treated early, before advanced scarring develops in the central macula, the prognosis for vision is generally good.
For more information about other inflammatory conditions and retinal diseases we treat, visit
tnretina.com/Treatment_&_Diseases_of_the_Retina
Information courtesy of ASRS Retina Health Series